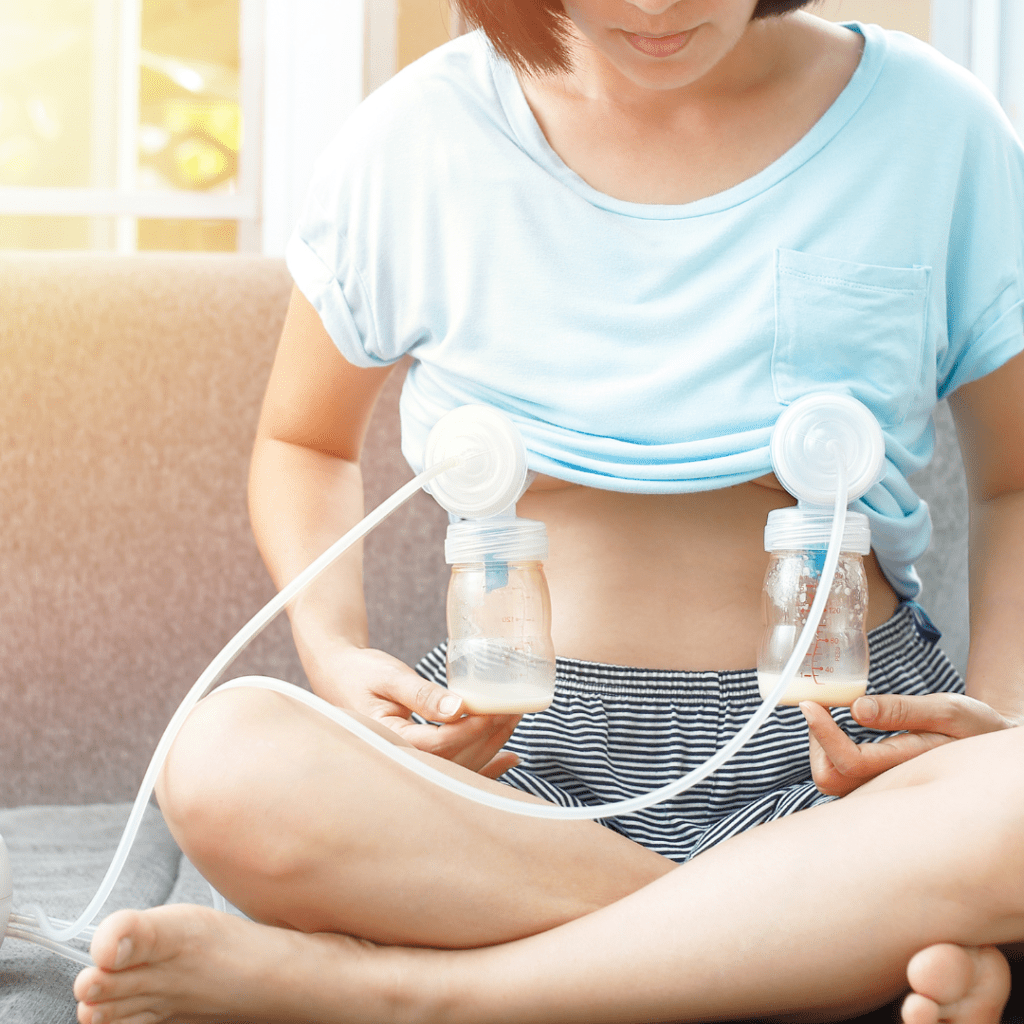
In hundreds of pumping consults and pump fittings, I have yet to meet someone who loved the experience of pumping. I’m sure they’re out there! But it’s certainly not a common phenomenon.
Most parents find pumping neutral at best, and annoying, uncomfortable, and/or painful at worst.
My goal as your pumping-savvy lactation consultant is to get pumping feeling as neutral as possible – maybe even rewarding. And most of the time, we can get there!
BUT in order to get there, we need to optimize a few things, including flange fit, choice of pump, and sometimes your body’s unique physiology.
Here are the most common reasons I see folks having a crummy time with pumping:
Reason #1: Pumping Hurts
Let’s say this loud and clear: PUMPING SHOULD NEVER HURT.
It should never hurt. Never!
According to pumping education queen Jeanette Mesite Frem: “Pumping should feel like nothing, or a gentle tug”. That’s it!
If you experience ANY of the following with pumping, you need to see a pumping-savvy IBCLC stat:
- pinching
- chafing
- pain (in nipple OR breast/chest)
- blisters
- blanching of the nipple afterwards (turning white)
- swelling of the areola
- recurring clogged ducts/mastitis
None of these should be happening.
Troubleshoot Painful Pumping
If pumping is painful, try these things:
- Decrease the vacuum level. Higher is not always better! Most people do not need the maximum setting to get their optimal milk output.
- Check your size – download my free nipple ruler to size yourself, or book a fitting with me or another experienced professional. Most people are not the size that comes in the box – and this can have a HUGE impact on comfort.
- Try lubrication – many people find that a little bit of coconut oil or pumping spray smeared inside the flange before starting can help quite a bit, especially if you have existing damage or inflammation from early nursing challenges or a poor flange fit.
If none of these fully resolve your discomfort, you may need professional support to get super precise with your flange size or try a different pump.
Reason #2: Pumping is Ineffective
Nothing is more disheartening than spending precious minutes hooked up to the pump, away from your baby, only to yield drops. I’ve sat with many clients who tearfully shared their frustration over spending hours pumping every day, yet still not meeting their milk production goals.
While pump settings & fit aren’t always the sole reason behind low milk production, they absolutely can be, and they are often the easiest intervention we can target right away.
All of the following can contribute to poor milk production when pumping:
- poor flange fit
- suboptimal pump
- incorrect settings
Troubleshoot Ineffective Pumping
If pumping isn’t yielding the output you want, try these things:
- Check your fit– download my free nipple ruler to size yourself, or book a fitting with me or another experienced professional. Most people are not the size that comes in the box – and this can make a big difference in output.
- Double check the settings. Do a quick search for your pump’s website (or a Youtube video from an IBCLC) walking you through the unique settings for your pump, and make sure you’re using it correctly.
- Try hands-on pumping. Did you know that gentle breast/chest massage while pumping can increase output by up to 50%? This can be really helpful to stimulate supply in the early weeks.
- Keep a consistent schedule. Milk production is a supply-and-demand system, which means we have to remove milk regularly to make milk. If you are exclusively pumping, you will likely need to pump every 3-4 hours (including overnight) to bring in a full supply at first.
- Try a different pump – if you’ve checked your fit, checked the settings, and tried hands-on pumping, and you’re still not producing your target output, you may need a different pump. Ask to borrow a tried-and-true workhorse pump (i.e. a Spectra S1 or S2) from a friend or colleague (you may need to purchase your own set of parts) and see if you notice a difference.
If you have tried all of the above but are still not meeting your output goals, it’s a good time to check in with an IBCLC for a comprehensive assessment for low milk supply. You may be doing ALL the things right, but your body may need additional support to make more milk. We have lots of tools in the toolbox for this!
Reason #3: An unchecked pumping aversion
Did you know that either D-MER (dysphoric milk ejection reflex) or nursing/pumping aversion are experienced by as many as 20% of lactating parents?
D-MER is a condition experienced by lactating parents where they experience abrupt feelings of sadness, dread, or anxiety before or during the letdown.
By contrast, aversion is when a parent experiences a negative feeling or sensation during nursing or pumping that isn’t limited to the letdown and often persists after the feeding/pumping session has ended.
These can have a significant impact on a parent’s desire to continue their lactation journey as well as their overall mental health, and warrant immediate care from a skilled IBCLC.
While we desperately need more data on these phenomena, I can report that anecdotally amongst my IBCLC colleagues, we consistently see a correlation between D-MER/aversion and imbalances in hormones and/or micronutrients.
Targeted support for these imbalances through strategic supplementation, mindfulness, and in some cases, medication, can be very effective at reducing symptoms.
Pumping Shouldn’t Suck
In short, pumping shouldn’t suck. It may not be a delightful, joyful, awe-inspiring experience – but it should at least be neutral and comfortable. You should be able to sit back and relax, scroll your phone, read a book, or watch a TV show while the milk is milking.
If you’ve tried the tips suggested here and are still struggling to get there with pumping, please don’t hesitate to reach out for support!


Leave a comment