One of the most misunderstood issues in infant feeding is food allergies.
Tell your pediatrician, your friends, or folks on social media that your baby is fussy, gassy, refluxy, or colicky, and often the first recommendation you’ll get is: have you tried cutting out dairy?
Cow’s milk protein allergy (CMPA) IS a fairly common occurrence in infants (reported as 2-7.5% prevalence) – but it is just one of the conditions that can cause fussiness, discomfort, and GI issues in babies. Other food sensitivities, oral dysfunction, gut dysbiosis, and others are also key players that are frequently missed and/or mistreated.
In this article, we’ll discuss why the tunnel vision on CMPA is letting families down, what the KEY symptom differentiators are, and how you can advocate for better care for your baby.
Mismanagement of Infant Food Allergies is Common
Oftentimes, when a parent’s dairy-free diet does not resolve symptoms in their nursing infant, or when a baby is fussy or has reflux on a lactose-based formula, providers will recommend switching to a hypoallergenic formula. In nursing dyads, this is NOT in the best interest of the parent or the baby, or in accordance with the official recommendations of the Academy of Breastfeeding Medicine. And in formula-fed babies, it often does not resolve symptoms or creates new or different symptoms.
In many such cases, CMPA is…
- not the correct allergy identified (baby is reactive to something else entirely, such as soy, gluten, or something else in parent’s diet)
- not the SOLE allergy identified (baby may be sensitive to multiple food proteins)
- not the correct diagnosis (baby doesn’t have an allergy at all, but rather another root issue causing symptoms)
- one of several root issues (baby has multiple layers of issues, and addressing one is not enough to see full resolution)
Before you get overwhelmed – these issues are often relatively simple to identify and/or treat! Working with a knowledgeable IBCLC can help. Keep reading to see what this process looks like.
If a parent who is nursing removes cow’s milk from their diet and does not see an improvement in symptoms within 3-7 days, then another approach to identify different or additional root causes needs to be considered.
In my practice, when a baby has major symptoms of food allergy or gut dysbiosis, we do the following:
- Identify the root cause(s) of the issue based on symptoms (and in some cases, testing)
- Incorporate effective, low-risk strategies for mitigating symptoms immediately
- Prioritize support for the parent’s mental health
- Collaborate on a short-term elimination diet (if indicated) to identify which food proteins triggering reactivity AND
- Implement a plan for gut healing for both parent & baby to improve symptoms & resilient wellness for the long term.
If a parent’s goal is to continue nursing, we prioritize that for BOTH the sake of parent’s desires & health AND the infant’s long-term gut health. If a baby is formula fed, then we work together to select an optimal formula.
Differentiating Between Food Allergy & Oral Dysfunction
In my experience, oral dysfunction is the alternate root cause most commonly missed by healthcare providers, and misdiagnosed as CMPA. There are other root causes of reflux, colic, and fussiness, but these two tend to be the most common, especially in the realm of feeding.
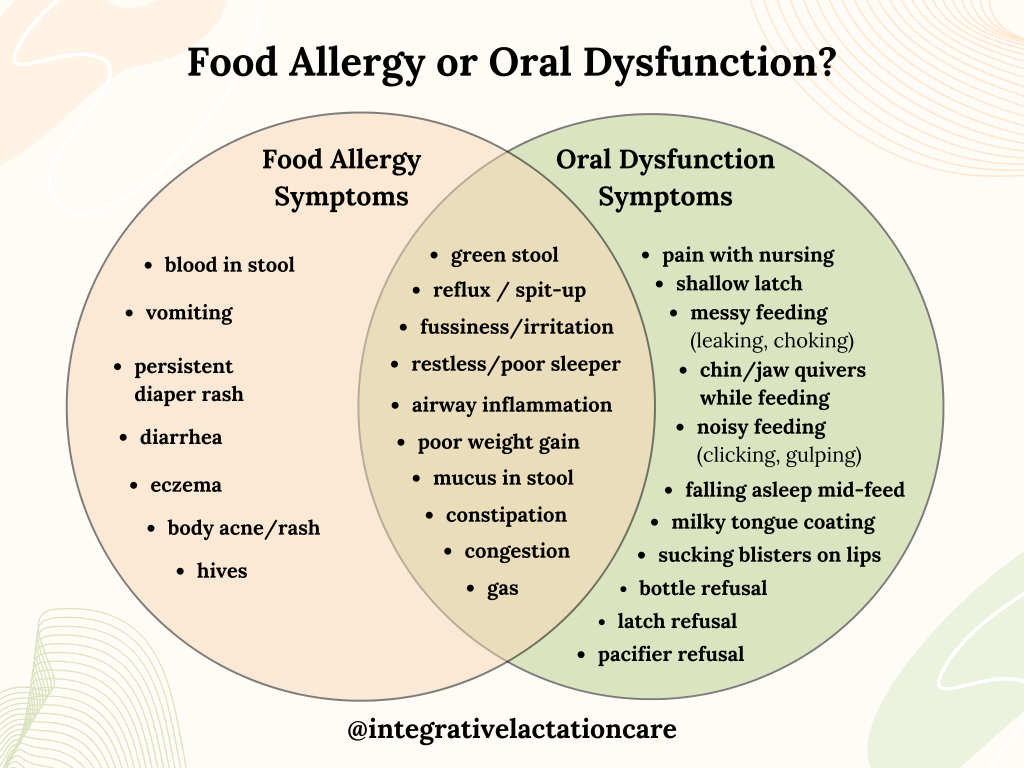
Distinguishing between infant food allergies and oral dysfunction can be challenging, as both conditions may present with overlapping symptoms. However, there are key differences in the signs and patterns of each condition that can help differentiate between the two. First, let’s clarify the symptom profile of each:
Food Allergy Symptoms
Symptoms can include:
- Gastrointestinal: Vomiting, diarrhea, blood or mucus in stool, constipation, reflux, or gas.
- Skin: Rash (including persistent diaper rash), hives, eczema, or in severe cases, swelling.
- Respiratory: Wheezing, coughing, nasal congestion, or difficulty breathing, particularly after eating.
- Systemic: Anaphylaxis (in severe cases) or general body tension from inflammation & discomfort.
- Feeding Behavior: The infant may show immediate discomfort, such as crying or irritability after ingesting certain proteins or foods.
- Stool: blood in stool, mucus in stool, green stool
Timing: In a nursing infant, timing of symptoms will vary based on when a parent consumes the allergen. Evidence suggests that proteins tend to peak in the nursing parent’s milk around 2-3 hours for cow’s milk, and other proteins studied are similar. Symptoms in the infant tend to be most significant immediately after feeding (either nursing or formula feeding).
Oral Dysfunction
Symptoms can include:
- Feeding Difficulties: Excessively long feeding times, leaking milk while feeding, frequent gagging, choking, or coughing during feeds, bottle refusal or bottle feeding difficulty.
- Nursing Issues: Pain with latching, bleeding or damaged nipples, shallow latch, difficulty latching.
- Poor Weight Gain: Inefficiency or fatigue during feeding can translate to insufficient intake (more prevalent in nursing).
- Oral Motor Issues: Weak or uncoordinated suck, poor lip seal, or difficulty protecting the airway, leading to swallowed air.
- Physiological Signs: Milky tongue coating, open mouth posture at rest, body tension, and/or recessed chin
- Stool: Mucus in stool, green stool, infrequent stooling/constipation
- Drooling: Excessive drooling (especially early on before teething is a factor) can be an indicator of poor oral function.
Timing: Symptoms tend to be consistent across feeding sessions (though may present differently in nursing vs. bottle). Sometimes issues are obvious from birth, though oral dysfunction frequently slides under the radar until 8-16 weeks, at which point factors such as suck reflex integration and milk supply regulation may reveal underlying difficulties.
Key Differentiators
If you read through both symptom profiles, you may have noticed that there are quite a few overlapping symptoms between food allergy and oral dysfunction.
Symptoms Common to Allergy & Oral Dysfunction:
- green stools
- reflux/spit-up
- fussiness, irritability, colic
- restless sleep or broken sleep
- airway inflammation
- congestion
- open-mouth breathing
- constipation (defined as anything less than DAILY stooling)
- gas
But there ARE standout symptoms that can help you determine which is the more likely root cause.

Unique Food Allergy Symptoms:
These symptoms are typically present ONLY in cases of an allergy (or occasionally, another source of gut dysbiosis).
- blood in stool
- vomiting or diarrhea
- persistent diaper rash
- eczema, body acne, or other skin rash
- hives or swelling
Unique Oral Dysfunction Symptoms:
These symptoms are typically present ONLY in cases of oral dysfunction.
- Noisy or messy feeding (clicking, coughing, gulping, leaking milk)
- Pain or damage from nursing
- Popping on/off while nursing
- Falling asleep mid-feeding (nursing or bottle)
- Milky tongue coating
- Chin/jaw quivering while feeding
- Sucking blisters or peeling on lips
It’s important to note that the presence of ANY standout symptom (even just one) is enough to pursue a formal diagnosis and specialized care. Your baby does not need to check every symptom on the list; most will present with some but not others.
What to Do:
If your baby has standout food allergy symptoms, I recommend working with a provider who has specific training & experience with babies with allergies and supporting infant gut health. Most pediatricians, lactation consultants, and even pediatric GI specialists do not have training in how to support the optimal health of the dyad. A holistic IBCLC (lactation consultant) or a functional/integrative pediatrician will be your best bet.
If your baby has standout oral dysfunction symptoms, I recommend working with an IBCLC or another infant feeding specialist who has specific training & experience with oral function & rehabilitation.
Most pediatricians & mainstream healthcare providers are not trained in identifying symptoms of oral dysfunction, and tend to automatically treat symptoms in the overlap category as either GERD or food allergy.
If this has been your experience, or you have otherwise struggled with colic, reflux, or food allergy, I’d love to hear about your journey here for a future blog post featuring parent stories.
Frequently Asked Questions:
Q: Is it possible for my baby to have standout symptoms of both food allergy and oral dysfunction?
A: Yes, it is absolutely possible – and it is why many parents who work really hard addressing one root cause still don’t see full resolution of symptoms.
Q: What if my baby doesn’t have any unique symptoms from either category?
A: If your baby ONLY has symptoms in the “overlap” list (i.e. reflux, general fussiness, etc), it will be particularly helpful for you to work with an IBCLC to identify the root cause. There are subtle differences in how those symptoms present, and having a full health history for you and your baby can help us discern how best to proceed.
Q: How do I find a provider who can help me get to the bottom of things?
A: There are an increasing number of functional/integrative providers who are committed to helping identify the root cause of health challenges & work towards full resolution of symptoms. I recommend asking around in your local parents group, or searching for a functional pediatrician in your closest metro area. Many IBCLCs (myself included) also offer virtual care.
Q: Does oral dysfunction mean that my baby has a tongue tie?
A: Possibly, but not necessarily. Oral dysfunction can happen for a variety of reasons, including restriction. You can download my free Oral Dysfunction Screening Tool to determine whether a comprehensive assessment for ties is indicated for your baby, and read my blog post on oral ties here.
Final Thoughts
It’s heartbreaking to see so many families pass through my practice who have weaned against their wishes, switched formulas 18 times, and/or trialed medication after medication, only to end up just as frustrated and exhausted as when they started. Parents deserve better guidance on navigating colic, reflux, and discomfort in their babies.
You have a right to advocate for supportive, knowledgeable care for your baby. If you have not been satisfied with the care you have received from your child’s healthcare provider, it is never to late to seek a second opinion or change providers. Your local parents’ group on Facebook may have helpful resources for other options to explore.
In the meantime, if you would like professional support ASAP to get to the bottom of your baby’s discomfort, you can book a virtual consult with me anytime.
Disclaimer: The guidance offered in this post is purely for educational purposes; it is not medical advice. Please consult your healthcare provider to explore your options for care.


Leave a comment