My primary motivation for becoming a lactation consultant was my own experience with my daughter’s oral ties when she was an infant. Since then, I’ve learned a great deal about oral dysfunction – and my goal in this piece is to clear up some of the rampant misinformation that’s I frequently see out there creating confusion for parents.
1 – Not all providers know how to properly assess for ties.
Most providers are not trained to perform a comprehensive assessment for oral ties. More than likely, they know how to recognize the most obvious presentation of a tongue tie (see below) but will frequently dismiss other presentations of oral restrictions, even when functional symptoms are present. It’s important to find a provider who is trained to perform a comprehensive assessment.

Pictured: An anterior tie with highly prominent tissue, which is generally the only type that most primary care providers will recognize and refer for treatment – despite the fact it is not the only type of restriction.
2 – A tie is defined functionally, not just anatomically.
The Academy for Breastfeeding Medicine defines ankyloglossia as “The presence of a sublingual frenulum that changes the appearance or function of the infant’s tongue because of its decreased length, lack of elasticity, or attachment too distal beneath the tongue or too close to or onto the gingival ridge.”
This means that a tie is not just defined by how the restriction appears in the infant’s mouth, but how that restriction affects function. In other words, if you are experiencing persistent issues with feeding that do not resolve with adjustments to latch and positioning, a tie may be the root cause.
3 – There is no such thing as a mild tie.
Since a tie is defined by a functional restriction, it stands to reason that there is no such thing as a mild tie. Either restriction that is impacting function is present, or it isn’t. Yes or no. Functional or not. There is no in-between. While there are a variety of ways that symptoms can present for a nursing dyad, and those may vary in severity, the presence of a tie means that dyad needs functional support. Whether that support ends up leading to a release of restricted tissue or assistance in helping baby manage compensations, strategic care is important. A family should never be dismissed from needing further support with the words: “it’s just a mild tie”. If you hear this, it’s a surefire sign you need a second opinion from a more qualified professional.
4 – A primary care provider (pediatrician, family doctor, midwife) should be looking at SYMPTOMS & referring to a specialist for care.
Since most primary care providers are not trained to complete a functional assessment for ties, the only care related to ties they should be offering you is a referral based on symptoms. Looking in your baby’s mouth isn’t necessarily going to be informative – but learning that your baby has reflux, slow weight gain, poor sleep patterns, and/or that the lactating parent has nipple pain and damage is very informative and warrants a referral to an IBCLC. If you’re experiencing these symptoms and your PCP hasn’t referred you to a lactation consultant, you might want to A. seek one out for yourself and B. let them know if the LC was, in fact, helpful. Maybe they will refer the next family with a similar symptom profile!
Furthermore, unless a PCP has specialized training in releasing oral ties, they should not be performing a frenotomy under any circumstances.
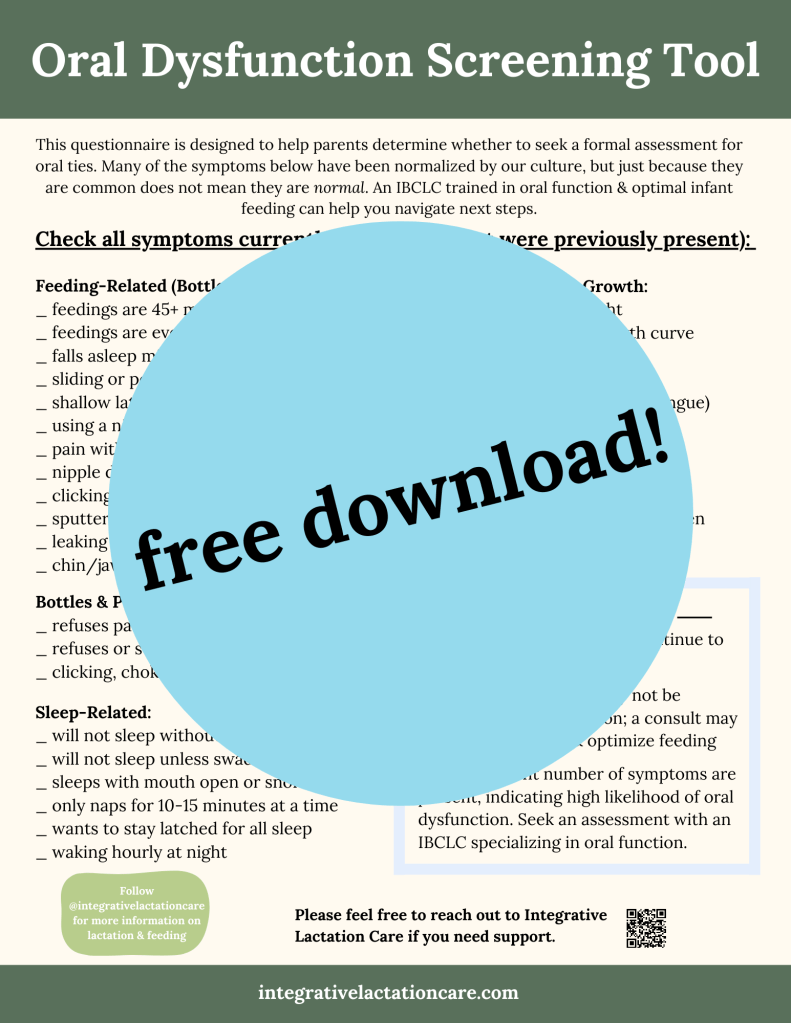
Are you a parent or a provider unsure if the symptoms you’re witnessing could be related to oral dysfunction or other treatable feeding issues?
Download my free screening tool here:
5 – Improving feeding via a release is a process, not a quick fix.
This is a critical one. Parents considering a tongue tie release often express concern over whether the procedure will be worth it because they have heard countless stories from peers or read on social media that they did not see improvement. In many cases, simply releasing restricted tissue may not enough to experience functional gains. You need to work with a provider who can support you before, during, and after the release. Of the families going through with a release procedure, very few are getting the support they need on the front and back end. Bodywork & oral rehabilitation with knowledgeable specialists are essential to an optimal outcome.
Too often, parents are relieved to finally have an explanation for their feeding struggles, and they jump straight to a release without taking the time to prepare and seek functional support. I know firsthand the desperation of struggling to feed your baby, and wanting to do the thing that will make it easier and better – but it is better to do it right and only have to do it once than have a suboptimal experience (and potentially have to do it over again in the future).
6 – The best place to start if you suspect ties is an infant feeding professional (ideally an IBCLC) with specialized training.
An IBCLC (International Board Certified Lactation Consultant) is the foremost expert on infant feeding and lactation. IBCLCs have a comprehensive understanding of a baby’s nutritional needs and how infant feeding is unique from that of older children/adults. They are uniquely positioned to support the breast/chestfeeding dyad, they understand the importance of treating two as one, and how anything you change on one side affects the other part of the dyad.
Specialized training is an important component here, because IBCLCs without additional education in oral dysfunction may not evaluate for ties any differently than the average PCP. While they may be well equipped to help a baby compensate more effectively through a better latch, or to help a parent protect their milk supply while supplementing, they may not have the skills to identify a functional restriction, differentiate a skilled release provider from an unskilled one, OR to support through the rehabilitation process.
Other providers such as OTs and SLPs may have a specialized skill set on the feeding and/or oral function front, but they usually do not have advanced training and education in lactation, or in working with newborns.
In general, an IBCLC who has taken specialized training in supporting families through the release process is your best bet for knowledgeable support. It is vital to work with a provider who can effectively assess what bodywork, oral exercises, feeding support, & other preparation your baby needs PRIOR to a release so that they can have the best outcome post-procedure.
7 – The skill and experience of the release provider is CRITICAL.
Any provider can purchase a laser and perform tongue tie releases; there is zero required training in order to be qualified to use a laser. Similarly, any ENT (or PCP) can pick up a pair of scissors and snip tissue. Just because a provider has the tool doesn’t mean they have the skills or experience to perform an effective, optimal release.
This is yet another reason why you’ll hear so many parents claiming that the release didn’t help their child – many release providers are performing incomplete or inadequate releases. Dr. Bobby Ghareri, an ENT who has performed over 13,000 releases and is one of the leading experts on tongue tie in the United States, says that if your baby had a scissor release while in the hospital, they are almost certainly still tied, because VERY few of those releases are skilled or complete.
Do you know what is one of the best indicators of a release provider who actually understands and cares about an optimal outcome? Whether they recommend (or require) you see a lactation/feeding professional and/or infant bodyworker prior to release.
Most tie-savvy IBCLCs have done their research to identify the best release providers in your local area and will be able to refer you to a trusted option or options. (I definitely have!)
8 – Doing aftercare – and the RIGHT aftercare – is VITALLY important.
Here’s another component of the process that is often forgotten, ignored, or mismanaged by providers who do not have appropriate training, and which leads to suboptimal outcomes for countless babies: AFTERCARE.
After a release, a new frenulum will form under the tongue in place of the old one. How the new tissue heals (and its degree of mobility) is highly dependent on how parents care for the wound. Performing effective & timely stretches around the clock, including overnight, for four weeks post-procedure is considered best practice for an optimal outcome.
Many families are given zero aftercare guidance, in which case the tissue may heal to be exactly as restricted as it was previously. Some families are given problematic aftercare guidance that is unnecessarily painful for baby and may create scar tissue. Sometimes, parents are given the correct exercises but not directed to do them often enough, and reattachment occurs.
In an ideal world, parents perform the correct exercises every 4-6 hours, including overnight, for four weeks. Optimal aftercare is vital to an optimal outcome.
Another vital component of aftercare is strategic rehabilitation. Babies form sucking patterns in utero, and if they have tethered oral ties, they have already been creating compensations for feeding before they were even born. Just because restricted tissue has been released does not mean a baby will be able to immediately feed effectively; in fact, most will need strategic support to make functional gains. This is why (per #6) working with a provider who has these specialized skills is recommended for an optimal outcome.
9 – Tongue ties impact more than just breastfeeding.
It is a common myth that tongue ties only affect breastfeeding, and that many children “grow out of them” and experience no other functional issues related to their health and well-being.
We have ample data confirming that tethered oral tissues (TOTs) affect everything from breast/chestfeeding AND bottle feeding to sleep, eating solid foods, speech, airway health, posture/alignment, digestive health, dental health, and more.
Every child is different and it’s impossible to know what the future holds for any individual – but as parents weigh the decision of choosing a frenotomy for their baby, they deserve to be informed about the long-term risks and benefits of both electing to do the procedure and electing not to do it.
You can read more here:
Long-Term Implications of Tongue Tie by Dr. Chelsea Pinto
Do Tongue Ties Affect Adults? by Dr. Richard Baxter
10 – Going through a release process isn’t easy – but if you have the right support, it can positively impact your child’s health for life.
No one likes the idea of their sweet baby having to undergo a procedure so shortly after arriving into the world. You had a vision of how you wanted to feed your baby, and most of us imagine it going with relative ease. It can be hard to adjust when reality is different from how you wanted feeding to go – and now you’re faced with the task of weighing the (often conflicting!) advice of different providers and considering a surgical procedure.
Especially if you’re in the early postpartum (but at any time as a parent), this can feel completely overwhelming. It’s enough to want to bury your head under the covers and ignore it completely – except that it’s affecting your baby’s ability to eat, so you can’t. It’s really hard; I know, I’ve been there.
You deserve to have compassionate, knowledgeable support to help you evaluate your options and support you through whatever decision you make and to an optimal outcome on the other side.
– Jill Mailing, IBCLC
Please feel free to reach out if I can help make your feeding journey easier!
or send a message: info@integrativelactation.com

References:
Academy of Breastfeeding Medicine Position Statement
on Ankyloglossia in Breastfeeding Dyads
Long-Term Implications of Tongue Tie by Dr. Chelsea Pinto
Do Tongue Ties Affect Adults? by Dr. Richard Baxter


Leave a comment